Image: Atomwise CEO and co-founder Abraham Heifets
Polio outbreak in New York state due to low vaccination coverage
New York has witnessed a polio outbreak due to low vaccination coverage, and GlobalData analysts say it needs to be addressed urgently.
Dr Judith M. Sills. Credit: Arriello
Dr Eric Caugant. Credit: Arriello
Poliovirus, the agent of poliomyelitis, has been detected in New York. The Rockland County Health Department reported poliovirus-positive samples from sewer district #1 in June 2022, followed by a case of paralytic poliomyelitis on July 21. The New York State Department of Health published regular updates, reporting that wastewater surveillance detected poliovirus in neighbouring Orange County in July and New York City in August. The presence of poliovirus marks the second outbreak of a highly infectious vaccine-preventable disease in the last four years in this region. GlobalData epidemiologists expect that areas with low vaccine coverage will experience poliovirus circulation and potential new cases until herd immunity is reached.
The presence of the virus in wastewater indicates that the virus is circulating in those communities. Poliovirus is mainly transmitted through the faecal-oral route, so consumption of contaminated food or water or contact with faeces can spread the virus. This also means that the virus sheds through faeces and can be found in wastewater.
All people infected with polio can spread the virus, regardless of symptoms. While many infected people will be asymptomatic, some may experience paresthesia (pins-and-needles sensations), and up to 25% of poliomyelitis cases will result in viral meningitis. Roughly 1 in 200 people with poliovirus will develop paralysis, which can be permanent. Paralytic poliomyelitis has a 2% to 10% mortality rate.
The burgeoning outbreak of polio is significant for two reasons: this is the first case of poliomyelitis in the US since 2013, and the population in which the virus is circulating is extremely vulnerable. The case occurred in an unvaccinated adult and has been determined to be a vaccine-derived strain. Cases of vaccine-derived polio can occur when there is insufficient vaccine coverage in an area, allowing the attenuated vaccine strain to develop gain-of-function mutations. This only occurs outside of the US, as the attenuated oral poliovirus vaccine (OPV) was replaced by the inactivated poliovirus vaccine (IPV) in 2000. Vaccinated persons are immune to both wild and vaccine-derived polio strains.
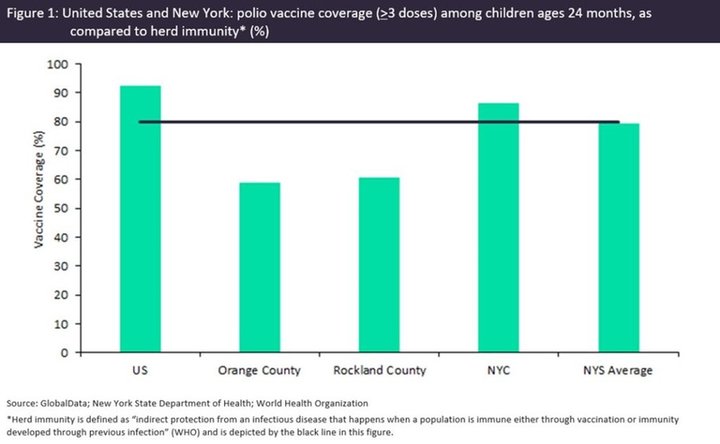
The World Health Organization (WHO) cites 80% polio vaccine coverage to achieve herd immunity, as indicated by the black line in Figure 1. Vaccine coverage in children ages 24 months in Rockland County, Orange County, and the New York State average all fall below this level at 60.34%, 58.68% and 78.96%, respectively. Low vaccine coverage allows the circulation of poliovirus in the community, endangering unvaccinated, immunocompromised, and other vulnerable individuals. In contrast, polio vaccine coverage (>3 doses) in the US general population is forecast to reach 92% in children ages 24 months by the end of 2022, according to GlobalData epidemiologists. However, actual vaccine coverage may fall slightly below forecast estimates due to the impact of the Covid-19 pandemic.
Vaccines